Diabetes mellitus and dentistry: the complications beyond the oral cavity
Diabetes mellitus (DM) is a chronic condition characterised by elevated blood glucose levels. Over time complications can develop such as damage to the heart, blood vessels, eyes, kidneys and nerves (WHO, 2021). The cause of elevated blood glucose is either an absence of insulin production, a lack of responsiveness to the actions of insulin, or some combination of both (Lamster, 2014).
The number of patients presenting to dental practices is continuing to rise amidst the increasing global prevalence which is estimated to reach 366 million by 2030 (Wild et al., 2004). In 2019, DM was directly responsible for 1.5 million deaths globally with nearly half (48%) occurring in people less than 70 years of age (WHO, 2021). Furthermore in 2015, the global economic cost for DM was US$1·31 trillion with indirect costs estimated to account for 34·7% of costs (Bommer et al., 2017).
The two main types of diabetes mellitus are type 1 and type 2 with the incidence of type 1 diabetes in the region of 15 per 100,000 people globally (Mobasseri et al., 2020) and a prevalence rate of 6059 cases per 100,000 for type 2 (Khan et al., 2020).
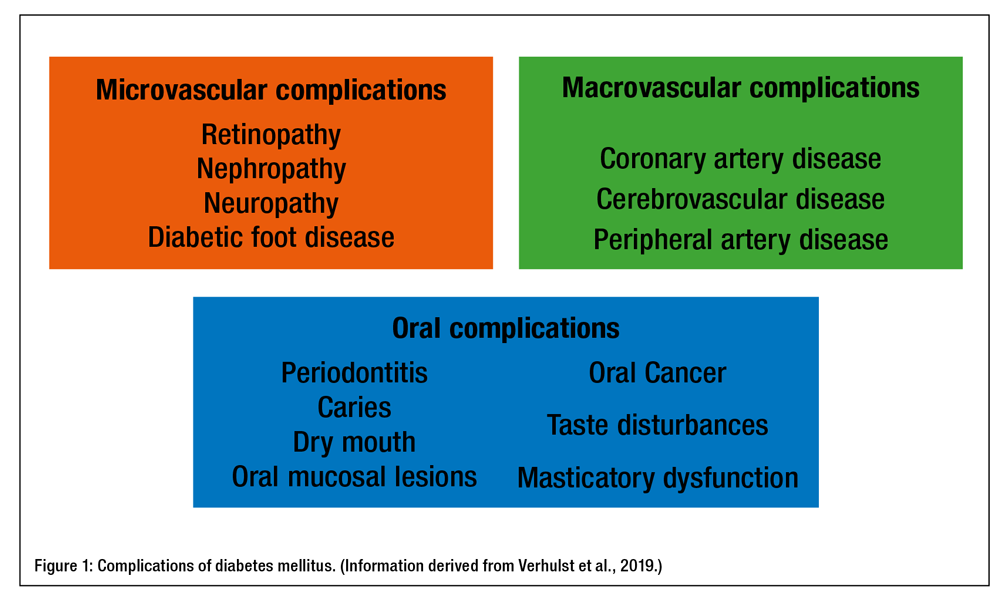
Diabetes mellitus results in multiple systemic complications as outlined in Figure 1.
As these startling statistics rise, are we prepared within diabetes dentistry for not only the oral complications of this chronic disease but also the physiological complications?
Complications of the disease other than oral manifestations which dentistry may face are outlined below.
Cardiovascular disease
Whilst type 2 diabetes and cardiovascular disease both increase with age (Chang and Halter, 2003) (Rodgers et al., 2019), treating patients with these conditions is extremely common in dental practice. Consideration must be given to patients with DM who may also be experiencing high blood pressure or other cardiovascular related ailments. Most dental professionals are highly experienced in management of patients with cardiovascular disease. However, some simple tips for considerations for management include:
- Recording the general medical practitioner details on the patient chart.
- Does the patient have their blood pressure checked regularly?
- Does the patient know what their normal blood pressure is?
- Does the patient get their cholesterol levels checked regularly?
- Has the patient had any cardiac interventions since the last visit or any changes to medication?
- Does the patient have any medication they take with them i.e., GTN spray for angina?
Nerve damage (neuropathy)
Neuropathy – damage or dysfunction to the nervous system – is considered the most common complication of diabetes resulting from long term poor management of blood glucose (CDC, 2021). It is estimated to affect nearly 50% of adults with diabetes during their lifetime (Hicks and Selvin, 2019). Oral manifestations often include a xerostomia, a subjective complaint of which the full pathological process is not fully understood but is believed to be related to elevated blood glucose (López-Pintor et al., 2016).
Furthermore, a recent cross-sectional study yielded results suggesting that sufficient chewing is imperative for successful diet therapy for diabetes and that long-term masticatory disorders are thought to be associated with the progression of diabetic condition. Findings showed that patients with type 2 diabetes who developed diabetic neuropathy had significantly reduced masticatory efficiency (Hamamoto et al., 2022).
Other considerations should be the access to the practice:
- Do patients have to climb stairs to reach the practice?
- Is there a falls risk due to neuropathy in a person’s feet as a result of diabetes?
- Is there a lift to get access if required?
- Highlighting vulnerable patients in advance of the appointment where possible and advising them to bring a chaperone if a patient reports unsteady on their feet.
Other dental considerations:
- If there is advanced neuropathy, can the patient feel the bristles on their gingival margins when brushing?
- Is the grip of holding the toothbrush affected? • Would they benefit from additional support such as a handle grip?
- Perhaps bringing a toothbrush along to dental hygiene visits would offer an opportunity to assess not only oral hygiene but the ability of the person with considerations given to the complications resulting from neuropathy in the mouth.
- Perhaps collaboration between dental professionals and dietitians is a future avenue to reduce complications at earlier stages if signs or symptoms are detected.
Kidney damage (nephropathy)
The prevalence of nephropathy in people with diabetes is thought to occur in 20% to 40% of all people with diabetes and can require dialysis and or transplantation (Gheith et al., 2016).
Kidneys are responsible for regulation of salt and water, excretion of metabolic waste products, different hormones and organic substances, and maintaining an acid balance. Therefore consideration must be given to treatment requirements and if the patient can undergo treatment in a local dental clinic or if they require referral to a specialist centre to manage their treatment needs. Dental management may need to be in collaboration with a specialist centre where complex needs present.
Eye damage (retinopathy)
One-third of adults with diabetes are affected by retinopathy and this is considered the leading cause of blindness in these individuals (Harding et al., 2018, Liew et al., 2017). Sight deterioration or blindness can lead to access issues for patients to find a new practice or find their way into a surgery.
Considerations to aid patients:
- Be mindful of possible sight problems amongst patients who may not wish to discuss it.
- Offering to assist a patient suspected of sight problems to the surgery can combat embarrassment for the patient.
- Other considerations include discussing the treatment plan verbally as well as giving a printed copy, so the patient has an opportunity to ask for clarification if unable to visually read the physical copy.
- If a person is nervous and has diminished sight it can be helpful to discuss the steps of a procedure so there are no sudden surprises and to alleviate anxiety.
Foot damage
The global prevalence of diabetic foot is 6.3% in people with DM (Zhang et al., 2017). It can lead to partial or full amputation of a person’s foot if resolutions do not occur. It was shown that prevalence increased with age, hypertension, diabetic retinopathy and a smoking history (Zhang et al., 2017). Diabetic foot disease can lead to issues with mobility if a person undergoes amputation and then requires a wheelchair.
Considerations for management:
- Does the practice have adequate wheelchair access facilities?
- Do reception staff triage a wheelchair patient’s needs on the phone prior to attendance?
- Can the patient transfer to the dental chair with or without assistance or does a chaperone need to attend to assist?
With the global prevalence of chronic systematic diseases rising, dentistry has a role to play in treating patients presenting with increasing medical complications. Education about common risk factors such as smoking and other lifestyle factors may be beneficial to reducing some elements of disease progression.
Practice protocols for the efficient management of such conditions, where possible, could save time and increase patient satisfaction as well as aiding treatment outcomes. Forecasting ways in which the patient visits can be deemed comfortable and minimising obstacles will enhance the delivery of care for patients and professionals alike.
 ABOUT THE AUTHOR
ABOUT THE AUTHOR
ÉILISH DUFFY
Éilish Duffy is a Clinical Educator for NSK with extensive experience of teaching Undergraduate Dental Hygiene and Dental Nursing Students in the UK and Ireland. She previously worked in research investigating oral bacteria and diabetic foot ulcers in patients with type 2 diabetes whilst also completing her MSc in Dental Hygiene through the Eastman Dental Institute, University College London. Presently, Éilish is a Lecturer in Dental Studies at the University of the Shannon, Midlands, and Midwest (TUS) and works in General Dental Practice.