Composite restorations and maintenance – before and after
Composite bonding is an increasingly popular cosmetic treatment for patients wanting to enhance their smile. This CPD article from Dental Therapist Lauren Long teaches you more about maintaining composite restorations to ensure patients’ smiles remain looking good for as long as possible.
The search for a ‘picture perfect’ smile continues to gather pace with increased patient demand for cosmetic dental procedures. While teeth whitening, veneers and crowns are probably the best known cosmetic treatments, there’s an increasing ‘buzz’ around composite bonding, something virtually unheard of a few years ago until it came to the attention of influencers on social media. Composite bonding is a relatively easy way to solve a range of minor dental problems. These include:
- Repairing chipped, fractured or broken teeth
- Closing spacing between teeth
- Covering minor discolouration
- Protecting areas of gum recession
The process involves adhering composite resin to a tooth which is then shaped and polished to restore its appearance. The resin is colour-matched to blend with the adjacent teeth so the restoration appears to be perfectly natural. It’s becoming a popular, cheaper alternative to crowns and veneers; a less invasive procedure, often without the need for injections and in many cases can be completed in a single appointment.
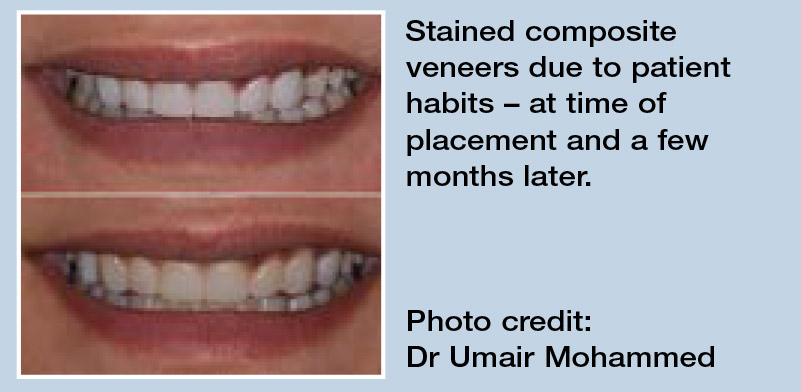
Poor polishing leads to staining
For patients who have had composite bonding treatment, or any type of composite restoration particularly in the aesthetic zone, good oral hygiene and regular hygiene therapy visits are essential. But how can we ensure that composite restorations remain looking good for as long as possible for our patients?
Much of this comes down to the polishing protocol used when restorations are placed. If they are poorly polished at this stage they will start to attract staining almost immediately after placement.
When a composite is light cured, the final layer – known as the oxygen inhibition layer – where oxygen interferes with the polymerisation of the composite, resulting in a sticky, uncured final layer – can quickly attract staining. To avoid this issue a final cure can be performed under glycerine gel. This results in a harder surface, that not only gives a better polish but is also more resistant to staining.
Polishing protocols
Spending plenty of time working through a meticulous polishing protocol will decrease the likelihood of staining. Everyone has their favourite polishing systems, tips and burs they like to use to create and maintain beautiful restorations. A smooth surface and high gloss is desirable not only for aesthetic reasons but also for good oral health as any rough surface is more likely to harbour biofilm, potentially causing periodontal issues.
However good the initial polishing, due to the inherent nature of composites, most will eventually attract some degree of staining. We can help our patients prevent this by encouraging them to lessen habits which cause composite staining, including:
- Smoking
- Heavy consumption of stain-inducing foods and drinks
- Use of abrasive toothpastes such as those containing charcoal
The properties of composite means the polish and shine will reduce over time. Patients should be advised before placement that they will need to have their bonding re-polished as and when required, generally around once a year.
Tackling staining
 When a patient presents with stained composite, there are many safe and effective ways we can remove this without affecting the integrity of the restorations. This can be done using high quality discs or wheels to restore shine and improve aesthetics while removing as little of the composite material as possible.
When a patient presents with stained composite, there are many safe and effective ways we can remove this without affecting the integrity of the restorations. This can be done using high quality discs or wheels to restore shine and improve aesthetics while removing as little of the composite material as possible.
If there is noticeable stain accumulating, the ideal and most gentle way to remove this is to use a glycine-based powder such as NSK Perio-Mate Powder. This fine, low-abrasive, water-soluble powder with a particle size of 23 microns, is safe to use on almost all tooth surfaces, including restorative materials as well as soft tissue.
I find this invaluable when a patient presents with stained restorations, especially in the aesthetic zone as their top priority is usually to restore their smile to its former glory by removing the discolouration that has accumulated. A glycine powder such as Perio-Mate Powder can achieve this gently and effectively without the worry of damaging any existing restorations they may have.
Gentle periodontal treatment
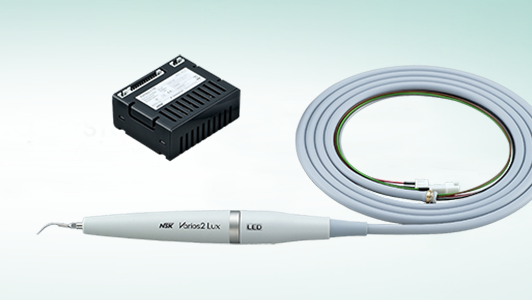
As well as stain removal, glycine is proven to be effective in removal of biofilm during supportive periodontal care and in maintaining implant health. Having the right oral hygiene equipment is essential in this role and this is why I constantly rely on my NSK Perio-Mate. I use the Perio-Mate to routinely support periodontal health and maintain my patients’ implants. Its ultra-fine water spray and powder team up to gently eradicate biofilm in as little as 20 seconds.
Alongside the Perio-Mate, I find my NSK Varios Combi Pro is the ideal way to combine ultrasonic scaling and powder therapy for more effective, comfortable and streamlined oral hygiene and biofilm control. The Varios Combi Pro automatically selects the functions for ultrasonic or powder therapy applications and has separate chambers for supragingival and subgingival powder. Separate handpiece hoses and handpieces also eliminates any risk of powder mixing or entering the control unit resulting in powder blockages.
The best patient outcomes
Always try to invest in the best equipment – it is a reflection on the work you do as an oral health professional. For me, equipment such as the Perio-Mate and Varios Combi Pro are essential tools to have in my surgery and can be used on almost every patient that I see.
Patients are always delighted with the outcomes of powder therapy, as well as loving the treatment process, which is comfortable, safe and effective with amazing results. With the right protocols in place, we can support our patients in achieving, and keeping a healthy, beautiful smile for many years to come.
 ABOUT THE AUTHOR
ABOUT THE AUTHOR
LAUREN LONG
Lauren Long is a Dental Therapist with over 10 years’ experience, who works exclusively in private practice in Edinburgh. Lauren is a Key Opinion Leader and Clinical Educator for NSK as well as Therapist Clinical Lead for Pain Free Dentistry Group. She has written articles for several publications and strives to support other Hygienists and Therapists in achieving the best possible working environment, whilst using their skills to create a career they love.